Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Key Takeaways
Morphine is a powerful opioid and carries a significant risk of addiction, as studies have shown.
Understanding how morphine affects the brain and body is crucial for both medical professionals and patients.
Early recognition and intervention are vital in preventing and treating morphine addiction.
Various treatment options, including medication-assisted treatment and counselling, are available for those struggling with addiction.
What is Morphine?

- Origin and History: Extracted from the seedpod of the opium poppy, morphine’s analgesic properties were discovered in the early 19th century.
- Medical Use: Primarily used to manage severe acute pain, such as post-surgical pain, and chronic pain in conditions like cancer.
- Mechanism of Action: It binds to opioid receptors in the central nervous system, reducing pain signals and the emotional response to pain.
- Risks: Despite its effectiveness, morphine has a high potential for abuse and addiction, necessitating strict medical supervision.
- Dual Impact: Morphine’s ability to alter pain perception and affect brain reward centres makes it a substance that must be used cautiously. Morphine abuse can lead to severe health impacts, including both physical and mental health dangers.
Morphine, a naturally occurring substance extracted from the seedpod of the opium poppy, has a long history in pain management. Dating back to the early 19th century, it was first isolated in 1804 and quickly became recognized over the counter for its effective analgesic properties. Its primary use is in the medical field, where it’s administered to treat pain and alleviate moderate to severe pain afterwards, especially following surgical procedures or in patients suffering from chronic pain conditions like cancer. Doctors carefully monitor prescribed morphine dosages to prevent dependence and misuse.
Morphine acts directly on the central nervous system. It binds to opioid receptors in the brain and spinal cord, effectively dampening the pain signals sent to the brain and other painkillers and reducing the emotional response to pain.
However, the use of morphine is a double-edged sword. While it’s unparalleled in its effectiveness against severe pain, its potential for abuse and addiction is high. The risk of addiction arises from the way morphine not only alters pain perception but also affects the reward centres of the brain. When morphine is regularly used over an extended period or in ways other than prescribed, it can lead to physical dependence and addiction. Thus, morphine must be administered under strict medical supervision, with careful monitoring for signs of dependency or abuse.
How Morphine Works
Morphine is a potent opioid pain medication that works by binding to specific receptors in the brain and spinal cord. These receptors, known as opioid receptors, play a crucial role in regulating pain, mood, and various bodily functions. When morphine binds to these receptors, it effectively blocks the transmission of pain signals to the brain, providing significant relief from moderate to severe pain.
Upon taking morphine, the drug is absorbed into the bloodstream and quickly distributed to the brain and spinal cord. Here, it attaches to the opioid receptors, which not only reduces the perception of pain but also triggers the release of dopamine. Dopamine is a neurotransmitter associated with feelings of pleasure and euphoria, which can lead to a sense of relaxation and well-being.
Morphine can be administered in various forms, including tablets, capsules, liquid, and injections. The method of administration and dosage will depend on the individual’s specific medical condition and needs. For instance, morphine tablets are commonly prescribed for ongoing pain management, while injections might be used for immediate pain relief in a hospital setting.
Understanding how morphine works is essential for both patients and healthcare providers to ensure its safe and effective use, particularly in managing severe pain.
Methods of Morphine Administration
Morphine can be administered in several ways, each having implications for its effectiveness, onset of action, and potential for misuse and addiction. Understanding these methods is crucial for medical professionals and patients to ensure safe and appropriate use. Here are the standard ways morphine is administered:
Oral Administration: This is the most common form of managing chronic pain. Morphine is available in tablets, capsules, and liquid form. Oral morphine has a slower onset but longer-lasting effects, making it suitable for long-term pain management.
Intravenous (IV) Injection: Used primarily in hospitals, IV injection delivers morphine directly into the bloodstream, providing rapid pain relief. This method is often used for acute pain management, such as post-surgical pain or severe injury. However, it has a higher risk for misuse and addiction due to the immediate and intense effects.
Intramuscular (IM) and Subcutaneous Injections: These methods involve injecting morphine into a muscle or under the skin. They have a slower onset of action than IV administration but are faster than oral forms. They are less common and are usually employed when IV access is unavailable.
Epidural and Spinal Administration: Morphine can be administered directly into the epidural or spinal space, providing significant pain relief during and after surgeries. This method targets the spinal cord’s pain receptors and effectively manages severe pain with less impact on the rest of the body.
Suppository: Rectal suppositories are another form of morphine administration used when oral intake is not possible. This method provides a slower release of medication and is less commonly used.
Transdermal Patch: Morphine can also be administered through a skin patch for continuous, slow release over several days. This method is typically used for chronic pain management in patients who require steady pain control.
Each method has its own set of advantages and risks. The choice of administration depends on the patient’s condition. The severity and type of pain often dictate what is needed. These can be broken down to the need for rapid onset, extended-release, or sustained release of the medication. It’s important for healthcare providers to choose the most appropriate method and monitor patients closely to prevent potential misuse and manage pain effectively. Individuals should take morphine as prescribed to ensure effectiveness and minimize the risk of addiction.
Managing Chronic Pain with Morphine
Morphine is often prescribed to manage chronic pain, which is pain that persists for more than three months and can be caused by conditions such as cancer, arthritis, and nerve damage. When used correctly, morphine can significantly improve the quality of life for individuals suffering from chronic pain.
Managing chronic pain with morphine requires a collaborative approach with a healthcare provider. This involves taking morphine as directed, regularly assessing pain levels, and adjusting the dosage as needed to achieve optimal pain relief. It’s crucial to follow the prescribed guidelines to minimize the risk of developing a dependency on the medication.
In addition to taking morphine, several strategies can help manage chronic pain effectively:
Relaxation Techniques: Practices such as deep breathing, meditation, and progressive muscle relaxation can help reduce pain and improve overall well-being.
Regular Exercise: Activities like walking, swimming, or yoga can strengthen muscles, improve flexibility, and reduce pain.
Healthy Lifestyle: Ensuring adequate sleep, maintaining a balanced diet, and staying hydrated can support overall health and pain management.
Heat or Cold Therapy: Applying heat or cold packs to the affected area can provide temporary pain relief.
Alternative Therapies: Treatments such as acupuncture, massage, or chiropractic care can complement traditional pain management strategies.
It’s important to be aware of potential side effects of morphine, such as constipation, drowsiness, and nausea. These can often be managed with additional medications or lifestyle adjustments. Always talk to your doctor about any side effects or concerns to ensure the best possible outcome in managing chronic pain.
How Does Morphine Addiction Develop?

- Initial Use: Often begins with a legitimate prescription for pain management.
- Alteration of Brain Chemistry: Morphine impacts the brain’s reward system by triggering dopamine release.
- Risk Factors: The risk of addiction increases with misuse, prolonged use, or higher doses.
- Tolerance Development: Regular use leads to tolerance, which then leads to requiring more of the drug for the same effect. Long-term morphine abuse can alter brain function and result in both physical and psychological dependence.
- Dependence and Addiction: Over time, dependence develops, characterised by a need to use morphine to feel normal and avoid withdrawal symptoms.
The journey from morphine use to addiction can often start innocently, typically with a legitimate prescription for managing pain. The initial use of morphine is generally safe when taken as directed by a healthcare professional. However, the risk of addiction emerges from the drug’s profound impact on brain chemistry.
When morphine enters the body, it binds to and activates opioid receptors located in the brain, spinal cord, and other organs. These receptors are part of the body’s pain-relief system and are linked to feelings of pleasure and reward. Activation of these receptors not only diminishes the perception of pain but also triggers the release of dopamine, a neurotransmitter associated with euphoria and well-being.
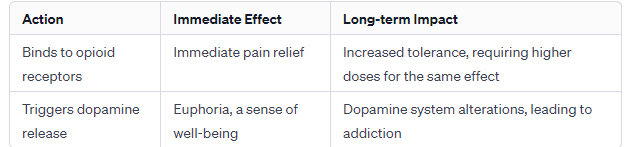
This release of dopamine can create a robust psychological response to relieve pain. For some individuals, the desire to recreate this euphoric sensation can lead to repeated misuse of pain relief medications such as morphine, even when the initial cause of pain has subsided. Over time, the brain starts to adapt to the presence of unwanted effects of the drug. It reduces the natural production of dopamine and increases the number of opioid receptors, leading to tolerance – where higher doses of pain medications or morphine are required to achieve the same effect.
As tolerance builds, dependence on prescription opioids can develop. Dependence on prescription medications is characterized by the need to continue using morphine to function normally and avoid withdrawal symptoms. It’s a significant step towards addiction – a chronic, relapsing disorder where the uncontrollable craving for the drug dominates an individual’s life, often at the expense of their health, relationships, and responsibilities.
Understanding the mechanisms of morphine addiction is crucial for both patients and healthcare providers. It highlights the importance of responsible prescribing practices, patient education, and early intervention strategies to prevent the transition of taking morphine from legitimate use for cancer pain to addiction.
Effective Morphine Addiction Treatment Options
Effective morphine addiction treatment involves several stages, beginning with medical detoxification to stabilize both mental and physical health, and requiring professional assistance due to potential health complications.
Morphine addiction treatment is a comprehensive process that includes detoxification and therapy to address both physical and psychological dependencies on the drug. It’s crucial to tailor these treatments to fit the unique needs of each individual. It takes into account factors like the severity of addiction, personal health history, and the presence of any co-occurring mental health disorders.
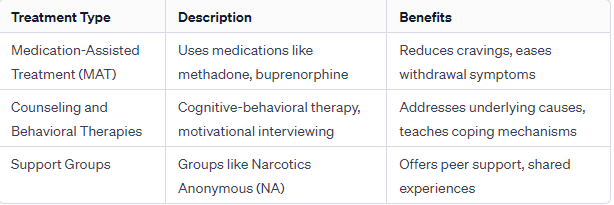
Medication-Assisted Treatment (MAT)
MAT combines medications with counselling and behavioural therapies. Medications used in MAT for morphine addiction include:
Methadone: Reduces withdrawal symptoms and cravings.
Buprenorphine: Lessens the effects of physical dependency.
Naltrexone: Blocks the euphoric effects of opioids. These medications help to normalize brain chemistry, block the euphoric effects of opioids, relieve physiological cravings, and stabilize body functions without the harmful effects of the abused drug.
Counselling and Behavioural Therapies
These are essential for addressing the psychological aspect of addiction:
Cognitive-Behavioral Therapy (CBT): Helps patients recognize, avoid, and cope with situations where they are most likely to use drugs.
Motivational Interviewing: Focuses on the patient’s readiness to change their behaviour and enter treatment.
Contingency Management: Uses a voucher-based system where patients earn points based on negative drug tests, which they can exchange for items that encourage healthy living
Support Groups and Peer Support
Engaging in support groups like Narcotics Anonymous (NA) or other community support groups can provide invaluable emotional and moral support. They offer a platform for shared experiences, coping strategies, and mutual encouragement.
Inpatient or Residential Treatment
These programs offer intensive care and are particularly beneficial for those with severe addiction or co-occurring disorders. Patients stay at a treatment facility with 24-hour medical and emotional support.
Outpatient Treatment Programs: These are less intensive than inpatient programs and are suitable for those with mild addiction or as a step-down level of care after inpatient treatment. Patients can continue with their daily lives while attending scheduled treatment sessions.
Aftercare and Relapse Prevention: After the initial treatment phase, ongoing support is crucial for maintaining sobriety. This may include ongoing counselling, support group meetings, and lifestyle changes to avoid triggers.
Effective treatment for morphine addiction must be comprehensive and personalised. It should address all aspects of addiction, from physical dependence to psychological triggers, other medications, and other medications, to ensure the best chance for a successful recovery and a return to a healthy, drug-drink alcohol-free life.
Recognising the Signs of Morphine Addiction
Early identification of morphine addiction is crucial for effective intervention and treatment. The signs of addiction to morphine can often be subtle and easily overlooked, especially in the early stages. However, as the addiction progresses, these signs become more pronounced and have a more significant impact on the individual’s life. Key indicators include:
Development of Tolerance
This is often the first sign of addiction. Over time, the body becomes accustomed to the presence of morphine, necessitating larger doses to achieve the same pain-relieving or euphoric effects. This increase in dosage can escalate rapidly, signalling a growing dependency.
These occur when the body reacts to the absence of the drug after chronic use.
Common withdrawal symptoms include:
Physical Symptoms: These can range from mild to severe and may include muscle aches, sweating, abdominal cramping, nausea, and diarrhoea.
Psychological Symptoms: Anxiety, agitation, insomnia, and mood swings are common. In severe cases, individuals may experience depression and intense drug cravings.
Continued Use Despite Negative Consequences
This is a hallmark of addiction. Individuals may continue using morphine despite facing severe negative impacts on their health, relationships, employment, or legal standing.
Examples of this are:
Health Consequences: Deteriorating physical health, increased risk of overdose, and development of co-occurring mental health disorders.
Relationships and Social Life: Strained family relationships, loss of friendships, social isolation, and neglect of social and familial responsibilities.
Work and Legal Issues: Decreased performance at work or school, job loss, financial difficulties, and potential legal issues related to drug possession or procurement.
Behavioural Changes: These can include secretive behaviour, changes in social circles, neglect of personal hygiene, and a lack of interest in previously enjoyed activities.
Increased Risk-Taking Behavior: Engaging in risky behaviours, such as driving under the influence or using morphine in dangerous situations, indicates a loss of judgment related to drug use.
Recognizing these signs is the first step in seeking help. Individuals and their friends and family need to be aware of these indicators. Early intervention can lead to more effective treatment outcomes and can significantly reduce the long-term consequences of addiction. They are continuing to use morphine despite harmful consequences to health, relationships, and daily life.
Summary
The essentiality of understanding morphine’s addictive potential cannot be overstated. Recognizing addiction signs early and seeking intervention are critical steps in addressing this challenge. Thankfully, with various effective treatment options available, overcoming morphine addiction is a realistic goal. The journey involves medical intervention, strong support networks, and a commitment to holistic recovery. Ultimately, the path to recovery, though demanding, paves the way for a healthier, more empowered life free from the constraints of addiction.
FAQs on Morphine Addiction
Is it possible to use morphine without becoming addicted?
While it’s possible, it requires careful monitoring and adherence to prescribed usage.
Can addiction develop even when morphine is taken as prescribed?
Yes, even when taken as prescribed, some individuals may develop an addiction.
What are non-opioid alternatives for pain management?
Alternatives include acetaminophen, NSAIDs, and certain antidepressants and anticonvulsants for neuropathic pain.
How can family members help someone with a morphine addiction?
Family members can offer support, get medical help, encourage treatment with other medicines, and participate in family therapy sessions.
Author
-
Dr Otulana is PCP’s longest-serving doctor. He is an experienced Physician with Specialist Interest in Substance Misuse Management and he has a wide range of experience in the assessment and management (including detoxification) of clients with various drug and substance addiction problems. Dr Otulana started practising as a doctor in 2000 and with over 10 years as an Addiction Physician. He is an Advanced Addiction Practitioner Member of Addiction Professionals and also holds the Certificate in Clinical Psychopharmacology (Part 1) of the British Association for Psychopharmacology. He is additionally a strong healthcare services professional with a Master of Business Administration (M.B.A.) degree from Cambridge University Judge Business School.
View all posts








